- The diagnostic value of circulating tumor DNA in hepatitis B virus induced hepatocellular carcinoma: a systematic review and meta-analysis
-
Young Chang, Soung Won Jeong, Jae Young Jang, Hyuksoo Eun, Young‑Sun Lee, Do Seon Song, Su Jong Yu, Sae Hwan Lee, Won Kim, Hyun Woong Lee, Sang Gyune Kim, Seongho Ryu, Suyeon Park
-
J Liver Cancer. 2022;22(2):167-177. Published online September 29, 2022
-
DOI: https://doi.org/10.17998/jlc.2022.09.19
-
-
2,603
Views
-
73
Downloads
-
1
Citation
-
 Abstract Abstract
 PDF PDF Supplementary Material Supplementary Material
- Background/Aim
New biomarkers are urgently needed to aid in the diagnosis of early stage hepatocellular carcinoma (HCC). We performed a meta-analysis on the diagnostic utility of circulating tumor DNA (ctDNA) levels in patients with hepatitis B virus-induced HCC.
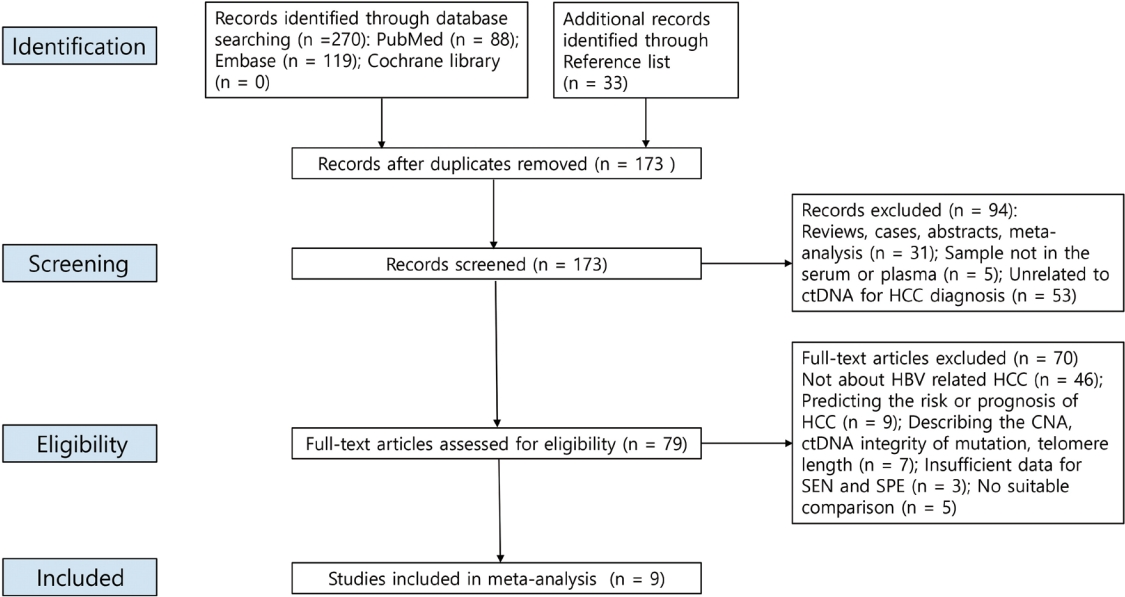
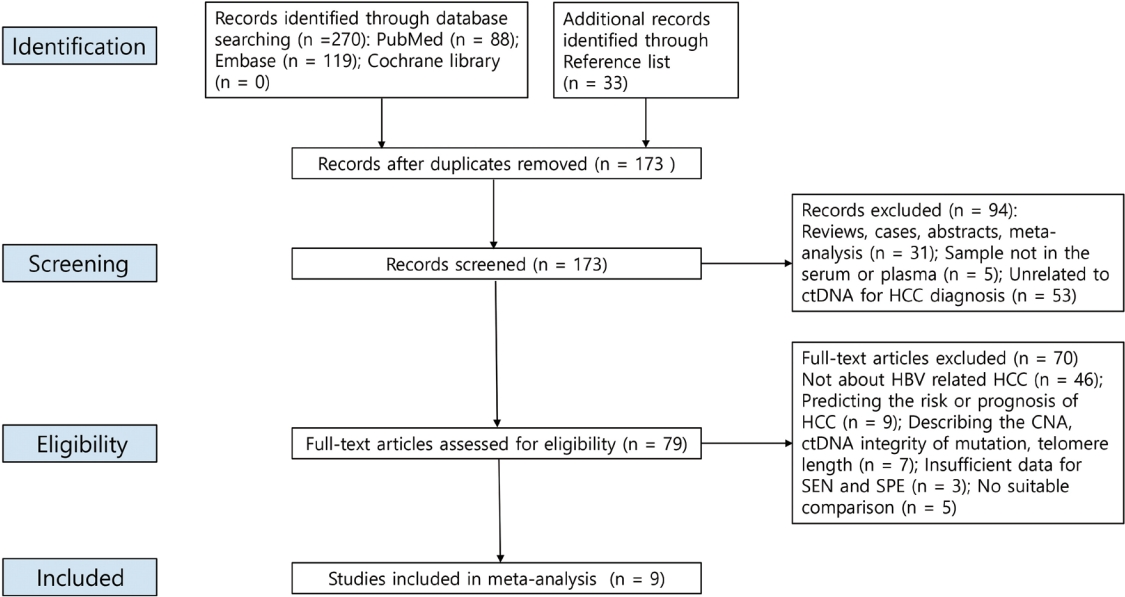
Methods
We retrieved relevant articles from PubMed, Embase, and the Cochrane Library up to February 8, 2022. Two subgroups were defined; one subset of studies analyzed the ctDNA methylation status, and the other subset combined tumor markers and ctDNA assays. Pooled sensitivity (SEN), specificity (SPE), positive likelihood ratio (PLR), negative likelihood ratio (NLR), diagnostic odds ratio (DOR), and area under the summary receiver operating characteristic curve (AUC) were analyzed.
Results
Nine articles including 2,161 participants were included. The overall SEN and SPE were 0.705 (95% confidence interval [CI], 0.629-0.771) and 0.833 (95% CI, 0.769-0.882), respectively. The DOR, PLR, and NLR were 11.759 (95% CI, 7.982-17.322), 4.285 (95% CI, 3.098- 5.925), and 0.336 (0.301-0.366), respectively. The ctDNA assay subset exhibited an AUC of 0.835. The AUC of the combined tumor marker and ctDNA assay was 0.848, with an SEN of 0.761 (95% CI, 0.659-0.839) and an SPE of 0.828 (95% CI, 0.692-0.911).
Conclusions
Circulating tumor DNA has promising diagnostic potential for HCC. It can serve as an auxiliary tool for HCC screening and detection, especially when combined with tumor markers.
-
Citations
Citations to this article as recorded by  - 16S rRNA Next-Generation Sequencing May Not Be Useful for Examining Suspected Cases of Spontaneous Bacterial Peritonitis
Chan Jin Yang, Ju Sun Song, Jeong-Ju Yoo, Keun Woo Park, Jina Yun, Sang Gyune Kim, Young Seok Kim
Medicina.2024; 60(2): 289. CrossRef
- A Case of Hepatocellular Carcinoma with Pulmonary Metastasis Who Showed Complete Response by Cytotoxic Chemotherapy after Sorafenib Failure
-
Hwa-Sun Park, Jae Young Jang, Min Young Baek, Yong Kwon Kim, Hyun Jin Youn, Su Young Back, Soung Won Jeong, Sae Hwan Lee, Sang Gyune Kim, Sang Woo Cha, Young Seok Kim, Young Deok Cho, Hong Soo Kim, Boo Sung Kim
-
J Liver Cancer. 2017;17(1):72-76. Published online March 31, 2017
-
DOI: https://doi.org/10.17998/jlc.17.1.72
-
-
 Abstract Abstract
 PDF PDF
- Hepatocellular carcinoma (HCC) is the 2nd most common cause of cancer related death
in Korea and well-known malignancy with poor prognosis. Sorafenib is the first-line
molecular targeted agent in patients with extra-hepatic spread of HCC. However, complete
response is extremely rare in patients treated with sorafenib and the disease control rate
is only 43%. We report a 53-year-old man with advanced HCC with pulmonary metastasis
who showed complete response by cytotoxic chemotherapy with doxorubicin and
cisplatin with relatively tolerable adverse effects after failure of treatment with sorafenib.
- A Case of Surgical Resection in Hepatocellular Carcinoma with Pulmonary Metastasis
-
Woo Jin Jung, Jae Young Jang, Jun Seok Park, Hee Jeong Lee, Young Kyu Cho, Soung Won Jeong, Sae Hwan Lee, Snag Gyune Kim, Sang Woo Cha, Young Seok Kim, Young Deok Cho, Hong Soo Kim, Boo Sung Kim
-
J Liver Cancer. 2016;16(2):145-150. Published online September 30, 2016
-
DOI: https://doi.org/10.17998/jlc.16.2.145
-
-
 Abstract Abstract
 PDF PDF
- Hepatocellular carcinoma (HCC) is well known malignancy with poor prognosis, even after
resection of the primary tumor. Sorafenib is the first-line treatment in advanced HCC, but the
disease control rate of sorafenib is only 43%. Pulmonary metastasectomy in patients with
pulmonary metastasis from HCC has been reported to increase long-term survival compared
with systemic chemotherapy. Video-assisted thoracic surgery is considered a reliable
approach to the diagnosis and treatment of pulmonary diseases with low complication
rate. Pulmonary metastasectomy is not universally accepted because of frequent local
recurrence, an uncontrollable primary tumor, and frequent multiple pulmonary metastases
in HCC, but outcome of pulmonary metastasectomy and adjuvant sorafenib therapy has
not been studied. We experienced a patient who had advanced HCC with pulmonary
oligometastasis and received surgical resection of the metastatic pulmonary nodule and
sorafenib chemotherapy. In advanced HCC with pulmonary oligometastasis, surgical
resection of pulmonary metastasis and sorafenib chemotherapy should be considered.
- A Case of Management for Early Recurrence after Hepatic Resection for the Treatment of Small Hepatocellular Carcinoma
-
Kyung Woo Park, Young Seok Kim, Sang Gyune Kim, Soung Won Jeong, Jae Young Jang, Hong Soo Kim, Sae Hwan Lee, Boo Sung Kim, Jun Cheol Jeong, Min Hee Lee, Jae Myeong Lee, Hee Kyung Kim
-
J Liver Cancer. 2015;15(2):122-125. Published online September 30, 2015
-
DOI: https://doi.org/10.17998/jlc.15.2.122
-
-
 Abstract Abstract
 PDF PDF
- For a small hepatocellular carcinoma (HCC), liver resection shows most favorable outcome in
case
which liver transplantation is not available, although it has also substantial recurrence
rate. Here, we report a case of recurred HCC with multiple intrahepatic metastasis at 5 months
after surgical resection for small HCC was done. A 55-year-old man with chronic HBV infection
received subsegmentectomy for HCC less than 2 cm. A follow-up computed tomography (CT)
at 5 months from operation revealed that there were multiple enhancing nodules in entire
remnant liver. Intra-arterial injections of adriamycin mixed lipiodol and gelfoam particles were
instituted through hepatic artery. We assume that poorly differentiated cellular feature would
be attributable to this kind of very early and aggressive recurrence of HCC. (J Liver Cancer
2015;15:122-125)
- Follow-up of Hepatocellular Carcinoma After Transarterial Chemoembolization; The Concordance of Contrast Enhanced Ultrasonography and Lipiodol CT
-
Gene Hyun Bok, Soung Won Jeong, Jae Young Jang, Sae Hwan Lee, Sang Gyune Kim, Sang-Woo Cha, Young Seok Kim, Young Deok Cho, Hong Soo Kim, Boo Sung Kim
-
J Liver Cancer. 2014;14(2):115-119. Published online September 30, 2014
-
DOI: https://doi.org/10.17998/jlc.14.2.115
-
-
 Abstract Abstract
 PDF PDF
- Background/Aim
s: The aim of this study is to evaluate the concordance of contrast-enhanced
ultrasonography (CEUS) and lipiodol computed tomography (L-CT) for the assessment of
viable hepatocellular carcinoma (HCC) after transarterial chemoembolization (TACE).
Methods
We retrospectively reviewed the post-TACE CEUS and L-CT images of 65
consecutive HCCs in 41 patients to assess the presence of viable tumor tissue. Forty-seven
HCCs in 31 patients that underwent post-TACE L-CT within 4 weeks of the CEUS examination
were included. The degree of concordance between CEUS and L-CT and factors related to
concordance were analyzed.
Results
The overall concordance of CEUS and LDCT was 78.7% (37/47). The concordance with
L-CT for viable tumor and non-viable tumor tissue on CEUS was 95.2%, and 65.4% respectively
(P<0.013). Diffuse tumors had a tendency for non-concordance (P=0.066). Although 3 of 4
lesions located in the hepatic dome were non-concordant, the sample size was too small to
establish significance. The mean tumor size for concordant and non-concordant tumors was
2.9 and 3.0 cm, with no significant difference.
Conclusions
Although the concordance of CEUS and L-CT for viable tumor tissue was
high, the concordance for non-viable tumor tissue was relatively low. Prospective studies
using angiography as a gold standard should be performed in the future. (J Liver Cancer
2014;14:115-119)
- Occurrence Rates of Hepatocellular Carcinoma in Patients with Adefovir-rescue Therapy for Lamivudine-Resistant Chronic Hepatitis B
-
Jihyun Kim, Sae Hwan Lee, Kanghyug Choi, Yun Nah Lee, Soung won Jeong, Sang Gyune Kim, Jae Young Jang, Young Seok Kim, Hong Soo Kim, Boo Sung Kim
-
Journal of the Korean Liver Cancer Study Group. 2013;13(2):130-135. Published online September 30, 2013
-
DOI: https://doi.org/10.17998/jlc.13.2.130
-
-
 Abstract Abstract
 PDF PDF
- Background/Aim
s: Suboptimal virological response to adefovir (ADV) rescue therapy was commonly experienced in patient with lamivudine-resistant chronic hepatitis B. The aim of this study is to compare occurrence of hepatocellular carcinoma (HCC) of patients with adefovir rescue therapy to naïve patients with entecavir.
Methods
Electronic medical records of 156 patients with lamivudine-resistant chronic hepatitis B who treated with ADV and of 186 naïve-patients who received entecavir 0.5 mg, as control group, were reviewed retrospectively. Study subjects were matched using estimated propensity score and 107 matched subjects in each group were analyzed. Cumulative occurrence of HCC was evaluated during antiviral therapy and the association between clinical variables and development of HCC were analyzed using Kaplan-Meyer curve and risk factor for HCC was evaluated with Cox-proportional hazard model.
Results
Age, gender, Child-Pugh score, underlying cirrhosis, HBeAg, and HBV DNA level were not different in both groups, except treatment duration with ADV or entecavir (mean 52.6±17.5 vs 46.7±11.4 months, P=0.004). Cumulative virological response rates were 16% and 42% in patient with ADV rescue therapy and 68% and 85% in naïve-patients received entecavir at 1 and 3 years (P<0.001), respectively. HCC were diagnosed in 6 of 107 patients with lamivudine-resistance and 9 of 107 naïve-patients during follow-period and cumulative occurrence rates of HCC was not different between both group (P=0.308). Cumulative occurrence rates of HCC in total 214 subjects were 2.3%, 4.8%, and 9.6% at 1, 3, and 5 years, respectively. Age, underlying cirrhosis, and baseline HBV DNA level were associated with the occurrence of HCC, however gender, HBeAg status, ADV rescue therapy, and cumulative virological response were not correlated in univariate analysis. In multivariate analysis, age (P=0.008) and underlying cirrhosis (P=0.002) were independent risk factors for occurrence of HCC.
Conclusions
Long-term ADV rescue therapy in patients with lamivudine-resistant chronic hepatitis B did not increase the occurrence rates of HCC.
- The Comparison of Overall Survival between Child C with Early Stage HCC and Child A with Advanced Stage HCC
-
Eui Ju Park, Jae Young Jang, Soung Won Jeong, Jin Woo Choo, Jin Nyoung Kim, Soon Ha Kwon, Byoung Moo Lee, Sae Hwan Lee, Sang Gyune Kim, Sang-Woo Cha, Young Seok Kim, Young Deok Cho, Hong Soo Kim, Boo Sung Kim
-
Journal of the Korean Liver Cancer Study Group. 2013;13(2):136-144. Published online September 30, 2013
-
DOI: https://doi.org/10.17998/jlc.13.2.136
-
-
 Abstract Abstract
 PDF PDF
- Background/Aim
s: The prognosis of hepatocellular carcinoma (HCC) is affected by stage as well as liver function. We analyzed the survival outcome of early stage HCC in Child class C patients and advanced HCC in Child class A patients.
Methods
Among 453 HCC patients with good performance status, Group A included 33 consecutive Child class C patients with early stage (I, II) HCC, and Group B included 45 consecutive Child class A patients with advanced stage (III, IV) HCC. We investigated the clinical characteristics, cirrhotic complications, and prognostic factors related with survival in each group, and compared overall survival between two groups.
Results
Age, prothrombin time, total bilirubin and Model for End-Stage Liver Disease (MELD) scores were significantly higher in Group A. Male sex, platelet count, albumin, sodium (Na), hepatitis B virus, alpha fetoprotein (AFP) and portal vein thrombosis were significantly higher in Group B. Complications of cirrhosis such as variceal bleeding, ascites, and hepatic encephalopathy were increased in Group A (P<0.05). Patients with an elevated AFP (>400 ng/mL) tended to exhibit poor survival as it increased in Group A (P=0.084). MELD scores>15 (Hazard ratio[HR] 17.84, 95% confidence interval [CI] 3.70-85.93, P<0.001), stage IV (HR:3.27, 95% CI 1.10-9.75, P=0.033), and absence of HCC treatment (HR: 3.70, 95% CI 1.06-12.50, P=0.040) were independent poor prognostic factors in Group B. Median overall survival was 24.6 months (95% CI 10.6-38.4) for Group A and 13.5 months (95% CI 4.6-22.3) for Group B (P=0.278). In the HCC treatment group, there were no significant differences of median overall survival between Group A and Group B, respectively (27.1 vs. 15.7 months, P=0.338). In patients with conservative treatment, Group A and Group B had a significantly different median overall survival of 13.6 and 2.5 months, respectively (P=0.012). In patients of Group B, median overall survival was significantly higher in patients who received treatment of HCC compared to those who did not, respectively (15.7 vs. 2.5 months, P<0.001).
Conclusions
Overall median survival was not different between both groups. However, in Child class A patients with advanced stage HCCs, the cumulative median survival was higher in patients who received treatment of HCC compared to those who did not. Therefore, advanced stage HCC patients with good liver function should be considered for HCC treatments.
- A Case of Unresectable Hepatocellular Carcinoma Treated by Repeated Transcatheter Arterial Chemoembolization Using DC beads® Followed with Resection
-
Jeong-Yeop Song, Young Seok Kim, Jae Myeong Lee, Soo Ji Jin, Kyu Sung Choi, Yun Nah Lee, Sang Hyune Kim, Sung Won Jeong, Jae Young Jang, Sae Hwan Lee, Hong Soo Kim, Boo Sung Kim
-
Journal of the Korean Liver Cancer Study Group. 2013;13(1):65-69. Published online February 28, 2013
-
DOI: https://doi.org/10.17998/jlc.13.1.65
-
-
 Abstract Abstract
 PDF PDF
- In patients with unresectable hepatocellular carcinoma (HCC) and no anti-cancer treatment, the prognosis is quite poor. But in
some cases, repeated sessions of transcatheter arterial chemoembolization (TACE) reduce the tumor size even to resectable, and
post-TACE resection may prolong the survival time. We present a case of 50-year-old HBV carrier woman with abdominal
distension. The diagnosis was huge HCC with intrahepatic metastasis. Repeated intra-arterial injections of adriamycin mixed
lipiodol or DC beads® (100-300/300-500/500-700 μm, ©BIOCOMPATIBLES UK LTD) were instituted through ten sessions for
13 months. The tumor size became reduced with a partial response after 10th TACE and post-TACE resection was performed. No
visible HCCs and decreased tumor markers were noted on the examinations 3 months after the resection.
- A Case of Good Responsed Bile Duct Invasion of Hepatocellular Carcinoma on Cyberknife Therapy
-
Dae Han Choi, Jae Young Jang, Soung Won Jeong, Sae Hwan Lee, Sang Gyune Kim, Young Seok Kim, Hong Soo Kim, Boo Sung Kim, A ram Jang
-
Journal of the Korean Liver Cancer Study Group. 2013;13(1):70-73. Published online February 28, 2013
-
DOI: https://doi.org/10.17998/jlc.13.1.70
-
-
 Abstract Abstract
 PDF PDF
- Hepatocellular carcinoma (HCC) is one of the common tumor worldwide and recorded as third most common cause of
cancer-related deaths. Invasion of the portal and hepatic veins by HCC is common. But intrabiliary invasion is rare. Radiotherapy
(RT) is considered appropriate for unresectable, locally advanced HCC without extrahepatic metastasis. With the conventional
RT, it is not possible to deliver a high radiation dose to a treatment volume in a short time and narrow lesion. Recent technological
developments in radiation therapy, such as stereotactic body radiation therapy (SBRT), make it possible to deliver a substantial
dose of radiation to the tumor and avoid radiosensitive normal liver in the vincinity. We report a patient who were treated by
cyberknife therapy for bile duct invasion of progressing HCC despite of treatment.
- A Case of Refractory Hepatocellular Carcinoma Presented with Brain Metastasis
-
Eui Bae Kim, Soung Won Jeong, Jae Young Jang, Sae Hwan Lee, Sang Gyune Kim, Young Seok Kim, Hong Soo Kim, Boo Sung Kim, A ram Jang
-
Journal of the Korean Liver Cancer Study Group. 2012;12(2):151-154. Published online September 30, 2012
-
-
-
 Abstract Abstract
 PDF PDF
- Hepatocellular carcinoma (HCC) is the sixth most common tumor worldwide and the third leading cause of tumor mortality.
The majority of tumors are diagnosed when advanced and then a 5-year survival rate of HCC is below 5%. However, recent
progress in the diagnosis and treatment of HCC has made it possible for the patient to survive longer, and as a result, distant
metastasis from HCC has increased and attracted more attention than before. HCC can be metastasized to all organs through
blood and lymphatic channel. Of the various metastatic sites, the most common site is the lungs, followed by the lymph nodes,
musculoskeletal, adrenal and omentum. Also, spleen, small bowel, large bowel and esophagus can be invloved. Brain metastasis
can be occurred rarely, and then it is regarded to oncologic emergency. We report a patient who present with brain metastasis of
progressing HCC despite of treatment.
- A Case of Mechanical Obstruction after Radiofrequency Ablation of Hepatocellular Carcinoma
-
Ji Eun Lee, Jae Young Jang, Soung Won Jeong, Sae Hwan Lee, Sang Gyune Kim, Young Seok Kim, Young Deok Cho, Hong Soo Kim, Boo Sung Kim
-
Journal of the Korean Liver Cancer Study Group. 2011;11(2):195-198. Published online September 30, 2011
-
-
-
 Abstract Abstract
 PDF PDF
- Radiofrequency ablation (RFA) inducing of coagulation necrosis by using thermal energy via electrodes placed within the
tissue effectively controls hepatocellular carcinoma (HCC). RFA has been commonly applied as an alternative curative therapy
to surgical resection for small HCC due to effective local tumor control. Although the technique is considered relatively safe,
several major complications requiring hospitalization for treatment have been reported such as vascular thrombosis,
pneumothorax, pleural effusion, skin burn, hematoma, liver abscess and colon perforation. Most complications occur due to
thermal injuries to adjacent structures by RFA. The risk of bowel perforation has been observed only when the target lesion is
adjacent to a gastrointestinal lumen, but, mechanical obstruction is extremely rare. Therefore, we report a case of mechanical
obstruction after transaction of ileum secondary to RFA of HCC.
- Thrombotic Occlusion of Right Femoral Artery Developed during Intra-Arterial Chemotherapy Through Chemoport
-
Jae Pil Han, Young Seok Kim, Sae Hwan Lee, Soung Won Jeong, Sang Gyune Kim, Jae Young Jang, Hong Soo Kim, Jae Myeong Lee, Boo Sung Kim
-
Journal of the Korean Liver Cancer Study Group. 2011;11(2):199-202. Published online September 30, 2011
-
-
-
 Abstract Abstract
 PDF PDF
- Although chemotherapy may not play a central role in the treatment of hepatocellular carcinoma (HCC), it must be one of the
important possibilities of multimodal treatment for advanced HCC. Intra-arterial (IA) chemotherapy which can deliver high
concentration of drug to the tumor has been widely used in unresectable or intractable HCC. It seems to reduce the incidence of
systemic side effects and improve drug efficacy. For this therapy, catheter implantation is required to infuse anti-tumor drug.
Here, we report a case of patient with complication developed during IA chemotherapy for advanced HCC with portal vein
thrombosis.
- A Case of Multiple HCC with Decompensated Liver Cirrhosis Treated by Intra-arterial Chemotherapy
-
Yun Suk Shim, Sae Hwan Lee, Hong Soo Kim
-
Journal of the Korean Liver Cancer Study Group. 2010;10(1):49-51. Published online June 30, 2010
-
-
-
 Abstract Abstract
 PDF PDF
- Hepatocelluar carcinoma (HCC) is one of the cancers with poor prognosis as HCC develops on base of cirrhosis in
majority cases, which requires multidisciplinary approach. Hepatic arterial infusion chemotherapy (HAIC) allows for relatively
easy replenishment of administering agents into the hepatic artery and achieves higher intrahepatic concentrations. We report
a case of multiple HCC with decompensated liver cirrhosis treated by HAIC.
|